A newly reported study has identified a molecular mechanism by which some common chemicals found in skin creams and other personal care products can trigger allergic reactions in the skin. The results suggest that the way these components displace lipids in skin cells may explain how they cause allergic contact dermatitis (ACD), and also point at a potential way of treating the condition. “What we present here is a molecular missing link,” said D. Branch Moody, MD, a principal investigator and physician at Brigham and Women’s Hospital division of rheumatology, inflammation, and immunity, who is co-senior author of the team’s published paper in Science Immunology. “We questioned the prevailing paradigm that T cell-mediated allergic reaction is only triggered when T cells respond to proteins or peptide antigens. We find a mechanism through which fragrance can initiate a T-cell response through a protein called CD1a.”
Moody and colleagues at Brigham and Women’s Hospital, Columbia University Irving Medical Center, and Monash University, reported their findings in a paper titled, “Human T cell response to CD1a and contact dermatitis allergens in botanical extracts and commercial skin care products.”
The human immune system has evolved to protect the body against foreign microorganisms, but must also tolerate foreign environmental compounds, such as those in plants, and foods, the authors wrote. Industrialization over the last couple of hundred years means that the immune system is also bombarded with a wide variety of other chemicals to which we are commonly exposed, either through pollution, or through the intentional use of drugs, fragrances, cosmetics, and other consumer products, many of which are applied directly to the skin. “Failure of the immune system to tolerate drugs, cosmetics, and other skin products causes allergic contact dermatitis, a T cell–mediated disease with rising prevalence,” the team further commented. “Accordingly, the incidence of contact dermatitis has risen, especially in industrialized countries.”
An allergic reaction is triggered when the immune system’s T cells recognize a chemical as foreign. “Considerable evidence documents a role for αβ T cells in contact dermatitis, which is caused by delayed-type hypersensitivity reactions,” the authors noted. These delayed type—or type IV—allergic reactions are thus T-cell mediated, and are worsened after repeated exposure to allergens, the researchers noted. During the sensitization phase, naive T cells are activated in a process that involves Langerhans cells, which are immune cells in the skin’s outer layer, and dermal dendritic cells. Then, in the elicitation phase, T cells cause inflammatory reactions in the skin.
The process by which T cells recognize allergens is believed to occur through the major histocompatibility complex (MHC) paradigm, via which a protein effectively provides a docking stage for a peptidic allergen, which is then displayed on the cell surface to T cells. However, most known contact allergens are non-peptidic small molecules, cations, and metals, suggesting that atypical binding interactions independent of MHC may activate T-cell receptors. “Biologists’ views of T-cell response are strongly influenced by the known mechanisms by which T-cell receptors (TCRs) recognize peptide antigens bound to major histocompatibility complex I (MHC I) and MHC II proteins,” the scientists acknowledged. However, T cells do not directly recognize small chemicals, and research suggests that these compounds need to undergo a chemical reaction with larger proteins in order to make themselves visible to T cells. “Thus, the chemical nature of contact allergens does not match the chemical structures of most antigens commonly recognized within the TCR-peptide–MHC axis.” As study co-leader Annemieke de Jong, PhD, assistant professor of dermatology at Columbia University Vagelos College of Physicians and Surgeons, explained, “… many small compounds in skincare products that trigger allergic contact dermatitis lack the chemical groups needed for this reaction to occur. These small chemicals should be invisible to T cells, but they’re not.”
De Jong and colleagues suspected that CD1a, a molecule that’s abundant on Langerhans cells, might be responsible for making these chemicals visible to T cells. In the current study, conducted using human cells in tissue culture, the researchers found that several common chemicals known to trigger allergic contact dermatitis were able to bind to CD1a molecules on the surface of Langerhans cells, and activate T cells. First author, Sarah Nicolai, MD, a research fellow in medicine at Brigham, exposed T cells to material from skin patch testing kits used in allergy clinics and found that T cells responded to tree oil balsam of Peru, and farnesol, which are found in many personal care products, such as skin creams, toothpaste, and fragrances. The team further identified that it was the benzyl benzoate and benzyl cinnamate compounds within balsam of Peru that were directly responsible for stimulating the T-cell response.
Overall they identified more than a dozen small chemicals that activated T cells through CD1a. “Our work shows how these chemicals can activate T cells in tissue culture, but we have to be cautious about claiming that this is definitively how it works in allergic patients,” de Jong acknowledged. “The study does pave the way for follow up studies to confirm the mechanism in allergic patients and design inhibitors of the response.”
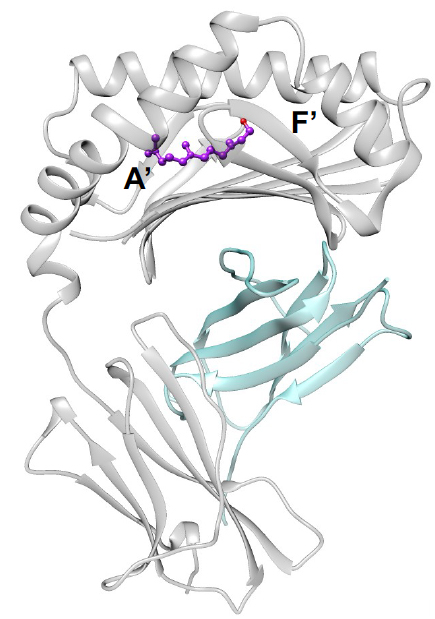
CD1a molecules normally bind the skin’s own naturally occurring lipids in its tunnel-like interior. These lipids protrude from the tunnel, creating a physical barrier that prevents CD1a from interacting with T cells. To further understand how these compounds triggered a reaction, investigators at Monash University carried out x-ray crystallography studies, which revealed that farnesol forms a complex with CD1a, and effectively kicks out naturally occurring human lipids, making CD1a more visible to T cells and leading to T-cell activation. Effectively, farnesol can hide inside the tunnel of CD1a, displacing the natural lipids that normally protrude from the CD1a molecule. “This displacement makes the CD1a surface visible to the T cells, causing an immune reaction,” de Jong said.
Currently, the only way to stop allergic contact dermatitis is to identify and avoid contact with the chemical that causes the reaction. Topical ointments can help soothe the rashes, and oral corticosteroids may be prescribed for severe cases, although these can increase the risk of infections and other side effects. The newly reported discovery raises the possibility that allergic contact dermatitis could be prevented by applying lipids to the skin that compete with and displace those triggering the immune reaction. “From previous studies, we know the identity of several lipids that can bind to CD1a but won’t activate T cells,” de Jong added.
The authors noted that while their work shows that fragrances found in personal care products can directly initiate a T cell response, further investigation will be needed to understand if this causes disease and allergic reactions. To better understand this, they will need to see if patients commonly have T cells that recognize molecules like farnesol. Nevertheless, as the authors concluded, “These studies identify molecular connections between CD1a and hypersensitivity to consumer products, defining a mechanism that could plausibly explain the many known T-cell responses to oily substances … The crystal structure of the CD1a-farnesol complex and study of the self-lipids bound to CD1a provided evidence for a molecular mechanism for recognition of a contact allergen, explaining how small antigens sequestered fully within CD1a can lead to T-cell responses through the absence of interference with CD1a-TCR contact.”
The team is also looking to find molecules that could feasibly block the response of CD1a and override the activation of T cells. Work is currently underway to identify promising molecules.
"Skin" - Google News
January 06, 2020 at 03:00PM
https://ift.tt/35m3LFK
Allergic Skin Reactions to Cosmetics and Perfumes Explained by Molecular "Missing Link" - Genetic Engineering & Biotechnology News
"Skin" - Google News
https://ift.tt/2Rv81zw
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
No comments:
Post a Comment